Facts to support your efforts to champion patient-provider communication
Even if you value being able to effectively support patients’ ability to summon help and communicate with caregivers, getting institutional buy-in and establishing a “culture communication” can be challenging. Making the case to staff and administrators will be more effective if you can marshall evidence based on data and regulatory requirements.
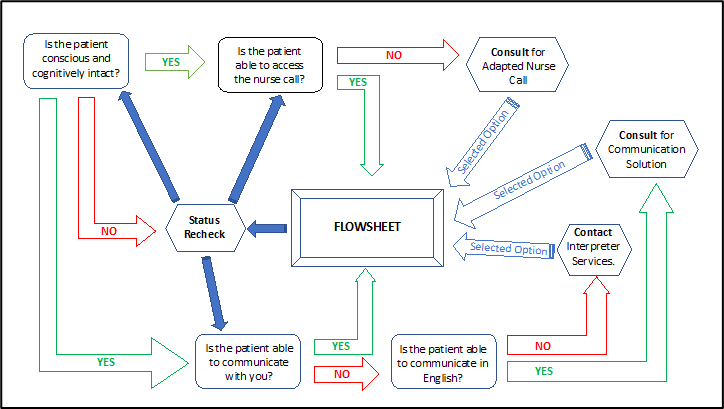
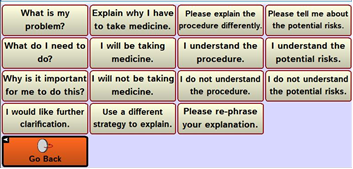
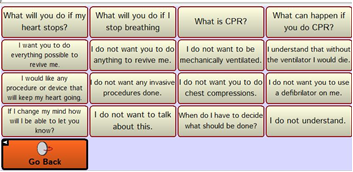
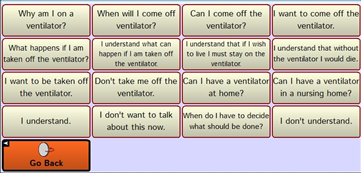
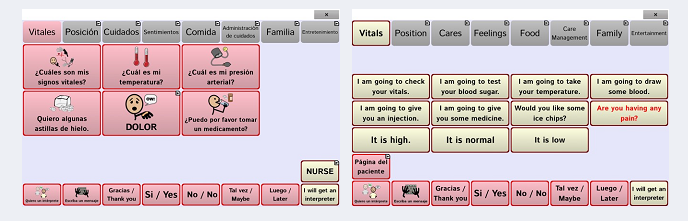
Sadly, patients who face barriers to effective communication are more likely to experience preventable adverse events that negatively impact their medical outcomes and land up costing hospitals billions of dollars. Some of the communication barriers are due to the patient’s medical condition while others may be due to a patient’s limited proficiency in the language spoken by the medical staff.
The impact and magnitude of such barriers are documented in a number of peer-reviewed papers that you can use in making your evidence-based argument for getting institutional buy-in to implement programs and strategies that allow patients to overcome communication barriers.
Agency for Healthcare Research and Quality. (2013b). Annual hospital-acquired condition rate and estimates of cost savings and deaths averted from 2010 to 2013. Rockville, MD: Author. Retrieved from https://www.ahrq.gov/professionals/quality-patient-safety/pfp/index.html
Bartlett, G., Blais, R., Tamblyn, R., Clermont, R. J., & MacGibbon, B. (2008). Impact of patient communication problems on the risk of preventable adverse events in acute care settings. Canadian MedicalAssociation Journal, 178(2), 1555–1562. https://doi.org/10.1503/cmaj.070690
Cohen, A. L., Rivara, F., Marcuse, E. K., McPhillips, H., & Davis, R. (2005). Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics, 116(3), 575–579. https://doi.org/10.1542/peds.2005-0521
Divi, C., Koss, R. G., Schmaltz, S. P., & Loeb, J. M. (2007). Language proficiency and adverse events in US hospitals: A pilot study. International Journal for Quality in Health Care Advance Access, 19, 60–67. https://doi.org/10.1093/intqhc/mzl069
Happ, M. B., Seaman, J. B., Nilsen, M. L., Sciulli, A., Tate, J. A., Saul, M., & Barnato, A. E. (2015). The number of mechanically ventilated ICU patients meeting communication criteria. Heart & Lung, 44, 45–49. https://doi.org/10.1016/j.hrtlng.2014.08.010
Hurtig, R., Alper, R. M, & Berkowitz, B., (2018) The Cost of Not Addressing the Communication Barriers Faced by Hospitalized Patients, Perspectives of the ASHA Special Interest Groups SIG 12, Vol. 3(3), 99-112. https://pubs.asha.org/doi/10.1044/persp3.SIG12.99
The Joint Commission. (2010). Advancing effective communication, cultural competence, and patient-and family-centered care: A roadmap for hospitals. Oakbrook Terrace, IL: Author.
The Joint Commission. (2011). Summary data of sentinel events reviewed by the Joint Commission. Oakbrook Terrace, IL: Author.
Zubow, L., & Hurtig, R. (2013). A Demographic Study of AAC/AT Needs in Hospitalized Patients. Perspectives on Augmentative and Alternative Communication, 22(2), 79-90. https://pubs.asha.org/doi/abs/10.1044/aac22.2.79
It is also important to make clear that statutory and accreditation standards require hospitals to address the access and communication barriers faced by their patients
Costello, J. M., Santiago, R. M., & Blackstone, S. W. (2015). Pediatric acute and intensive care in hospitals. In S. Blackstone,
D. Beukelman, & K. Yorkston (Eds.), Patient–provider communication in healthcare settings: roles for speech-language pathologists and other professionals. Plural.
Hurtig, R. R., Nilsen, M., Happ, E. B., & Blackstone, S. (2015).
Acute care/hospital/ICU adults. In S. Blackstone, D. Beukelman, & K. Yorkston (Eds.), Patient–provider communication in healthcare settings: Roles for speech-language pathologists and other professionals. Plural.
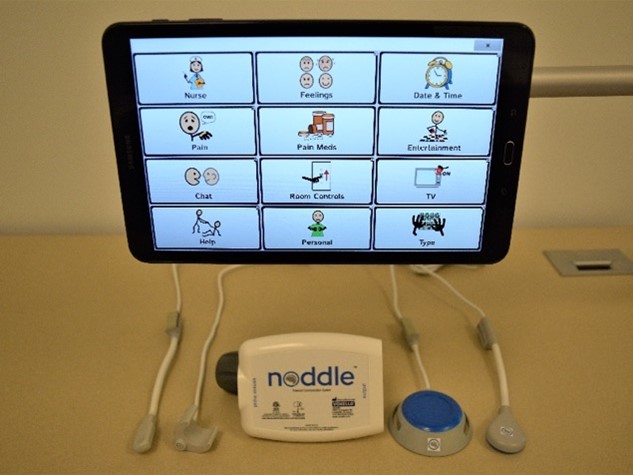
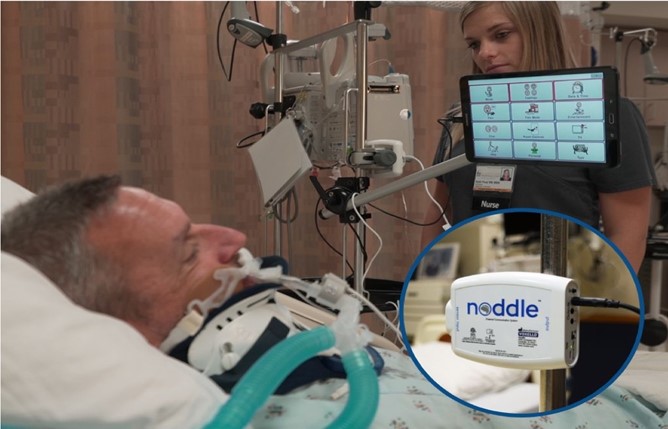
You can find out more about how Voxello supports patient-provider communication by visiting www.voxello.com.
Facts to support your efforts to champion patient-provider communication Read More »